What is biocompatibility? In brief, biocompatibility refers to the interaction of a material, known as a biomaterial, with a living organism, often referred to as a host. Put simply, biocompatible materials are those employed in medical devices that come into contact with or are placed within the human body.
Which materials — metal and polymer — are biocompatible? What does testing entail? When you are developing a product using biocompatible metals or polymers, what factors should be considered? Here is what you need to know.
DISCLAIMER: The following information is not medical advice. It was written for informational purposes only. If you have a medical question, please speak with your physician
Why Biocompatible Materials Are Essential for Patients’ Safety
Biocompatible materials are essential for patient safety in the medical field for several important reasons:

Prevention of Adverse Reactions
When medical devices or materials come into contact with the human body, there is a risk of adverse reactions if the materials used are not biocompatible. Adverse reactions can include inflammation, allergic responses, toxicity, and other harmful effects. Biocompatible materials are designed to minimize these risks and prevent harm to patients.
Minimizing Infection Risk
Biocompatible materials help minimize the risk of infections. Non-biocompatible materials may create sites where bacteria can thrive, leading to infections that can be challenging to treat and harmful to the patient.
Tissue Compatibility
Biocompatible materials are designed to interact harmoniously with surrounding tissues. They do not provoke excessive immune responses or tissue rejection, ensuring that the patient’s own body can accept and tolerate the medical device or material.
Compliance with Regulatory Standards
Regulatory bodies in various countries, such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), require that medical devices meet stringent biocompatibility standards. Compliance with these standards is necessary to gain regulatory approval and ensure that devices meet safety requirements. Only approved materials are recognized as safe, trustworthy, and fit for medical use.
Regulations for Biocompatible Materials
Materials used in medical devices are subject to the stringent quality and performance requirements of the international regulation ISO 10993, which deals specifically with biocompatibility, to ensure that medical devices, materials, and implants are safe for use in contact with the human body.
Biocompatibility is a complex and evolving subject. The latest update of the ISO 10993 guidance (10993-1:2018; updated from 10993-1:2009) reflects the latest developments in the field. This latest edition expands the standard’s scope to provide more detailed explanations and examples, offering clearer applicability to a broader range of medical devices and materials. It places a stronger emphasis on risk management as a fundamental step throughout the biological evaluation process, requiring manufacturers to create a “biological evaluation plan”. The introduction of a “biological evaluation plan” outlines the strategy for the evaluation, considering device characterization, intended use, patient population, and materials to guide the selection of specific tests and assessments. The standard underscores the importance of collecting information on materials and conducting chemical characterization to identify and quantify chemicals and potential impurities. This chemical data is crucial for determining the necessary biocompatibility tests.
ISO 10993-1:2018 also encourages the use of existing data, including information from predicate devices, historical data, and scientific literature, to support biocompatibility assessments, promoting efficiency and reducing the need for redundant testing. The standard provides comprehensive guidance on documenting the biological evaluation process, including the rationale for test selections, test results, and conclusions. Additionally, it addresses the assessment of material changes and manufacturing processes, ensuring that changes do not compromise biocompatibility.
Biocompatibility testing involves 3 types of test:
- Analytical Chemistry
- In vitro testing
- Animal testing
Considerations for Choosing Biocompatible Materials
When choosing biocompatible materials for medical devices or implants, there are several important considerations to take into account, here are key considerations for choosing biocompatible materials:
Material Availability
Material availability is a crucial consideration in the selection of biocompatible materials. It refers to the accessibility of the chosen material in terms of quantity, quality, and cost. Some materials may be rare, expensive, or have limited availability due to factors such as geographic sourcing or production limitations. When choosing materials, manufacturers must assess whether the chosen material can be consistently sourced in the necessary quantities to meet production demands, otherwise, an alternative solution may be necessary.
Manufacturability
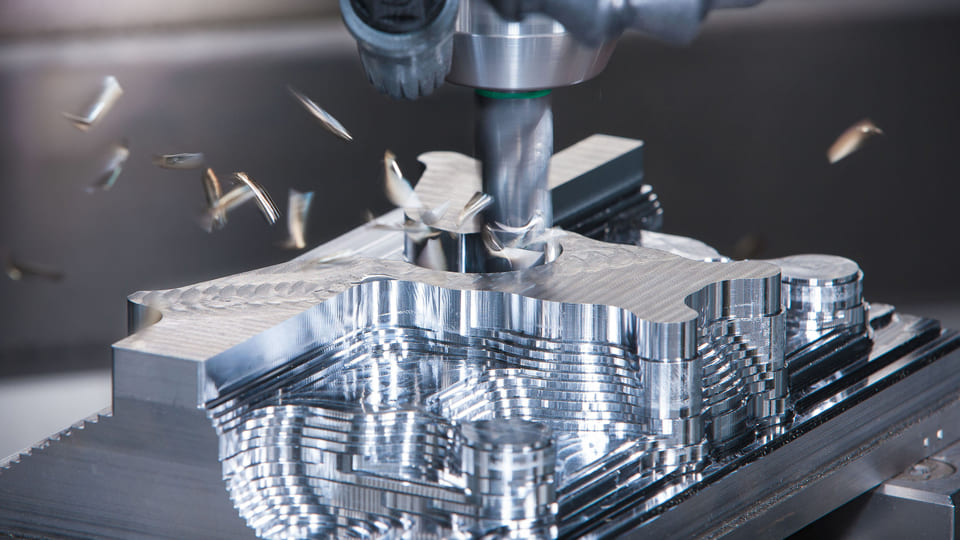
The manufacturability of a material is a key factor in determining its suitability for use in medical devices or implants. It encompasses a range of characteristics, including machinability, formability, and compatibility with various manufacturing processes. The chosen material should be amenable to processing, shaping, and assembly into the desired medical device while maintaining its structural integrity and biocompatibility.
Injection molding is a highly efficient method for producing large quantities of precise plastic components with excellent surface finishes, making it ideal for high-volume production. However, it can be cost-prohibitive for small-batch production. CNC machining offers great versatility in terms of materials but has limitations in machining complex geometries. Additive manufacturing technologies are revolutionizing production by enabling faster and more customized output, a valuable feature in light of the medical sector’s shift towards patient-centric care. It’s important to note that both CNC machining and additive manufacturing have constraints when it comes to material options.
Related resource: Plastic Injection Molding in The Medical Industry
Reprocessing and Sterilization
Reprocessing and sterilization are critical aspects of using medical devices, and materials must be able to withstand these procedures without compromising their biocompatibility and performance. Medical devices are often subject to rigorous sterilization processes, including autoclaving, ethylene oxide gas sterilization, or gamma radiation. Materials that degrade, corrode, or lose their structural properties under these conditions are unsuitable for medical applications.
Sustainability
In recent years, sustainability has become an increasingly important consideration in material selection for medical devices. Sustainability involves evaluating the environmental impact of materials, considering factors such as biodegradability, recyclability, and energy efficiency in production. Sustainable materials are preferred to minimize waste, reduce energy consumption, and lower the carbon footprint associated with the manufacturing and use of medical devices.
Types of Biocompatible Materials
Biocompatible materials used in the medical field come in a variety of forms to meet the specific needs of different medical devices and applications. Here are some common types of biocompatible materials:
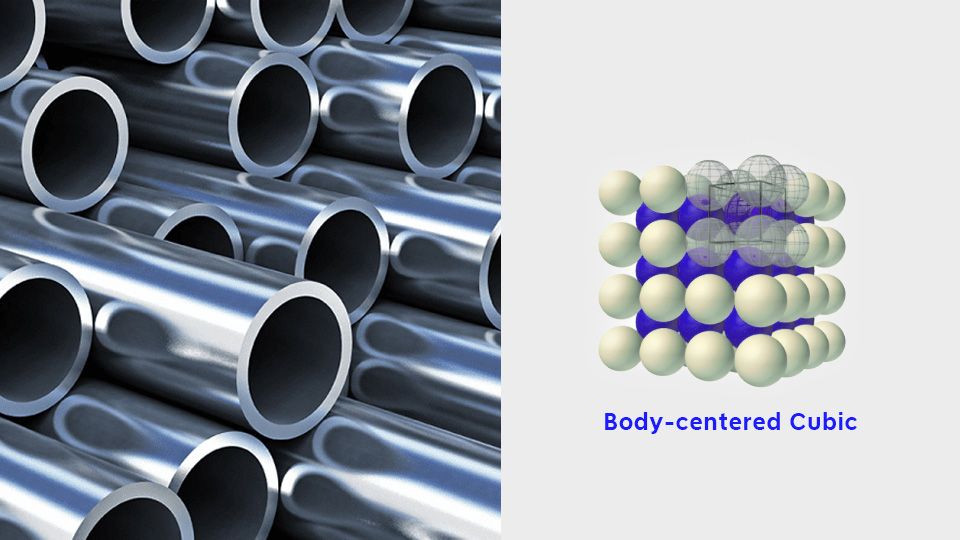
Metals
Stainless Steel: Often used in surgical instruments and orthopedic implants due to its strength, corrosion resistance, and durability.
Titanium: Widely employed for dental implants, artificial joints, and orthopedic devices because of its biocompatibility and lightweight, corrosion-resistant properties.
Cobalt-Chromium Alloys: Suitable for orthopedic and cardiovascular implants due to their strength and wear resistance.
Polymers
Polyethylene(PE): Used in joint replacements and prosthetic devices due to its low friction, durability, and biocompatibility.
Polylactic Acid (PLA): Biodegradable and used in absorbable sutures and drug delivery systems.
Poly(methyl methacrylate) (PMMA): Used in bone cement for joint replacements.
Ceramics
Alumina (Al2O3): Employed in ceramic hip replacements and dental implants for its biocompatibility and wear resistance.
Zirconia (ZrO2): Used in dental implants and orthopedic applications for its high strength and biocompatibility.
Hydroxyapatite (HA): A component in coatings for orthopedic and dental implants to enhance bone integration.
Medical-grade Silicone
Used in a wide range of medical devices, such as catheters, breast implants, and facial prosthetics, due to its flexibility and biocompatibility.
Bioglass
Bioglass is a bioactive glass that can bond directly with living tissues and promote tissue regeneration. It is often used in the development of dental implants, bone grafts, and other medical devices, thanks to its ability to facilitate the integration of synthetic materials with natural body tissues.